March is Endometriosis Awareness Month. Endometriosis is an inflammatory condition where endometrial tissue (tissue similar to the lining of the uterus) grows outside of the uterus. It is estimated that 1 in 10 women have endometriosis (Zondervan 2020).
Endometriosis frequently presents with the symptom of pain including dysmenorrhoea (painful periods), dyspareunia (pain during sexual intercourse), and chronic pelvic or abdominal pain.
Endometriosis can cause infertility and for women with subfertility the prevalence rate ranges from 25% to 40% (Ozkan 2008). In February 2022, the European Society of Human Reproduction and Embryology (ESHRE) published an updated Guideline on Endometriosis, including information for patients.
Cochrane Gynaecology and Fertility group has published over 20 intervention reviews and protocols investigating the effectiveness and safety of treatments for the management of endometriosis. In addition, we have published five diagnostic test accuracy reviews assessing the effectiveness of various tests in the diagnosis of endometriosis. We are joining #EndometriosisAwarenessMonth campaign by sharing our updated Cochrane review collection on endometriosis. The reviews focus on pain-related outcomes as well as fertility outcomes. The interventions include medical treatment (hormonal therapy, immune-modulators, anti‐inflammatory drugs), surgery, and alternative medicine.
Endometriosis: Collection of Cochrane Reviews
Endometriosis: an overview of Cochrane Reviews
This overview published in 2014 summarised the evidence from Cochrane systematic reviews on treatment options for women with pain or subfertility associated with endometriosis. The overview included reviews pain relief (14 reviews) as well as review reporting fertility outcomes (8 reviews).
Pain relief

Medical treatment
Danazol is a hormone that produces male characteristics as well as weight gain and acne. It may, however, relieve the painful symptoms of endometriosis, although the side effects can be unacceptable (such as acne or muscle cramps). Treatment with danazol appeared to be effective in relieving painful symptoms related to endometriosis when compared to placebo. The improvement was still present six months after treatment was stopped. There was some evidence that women who took danazol were satisfied with the treatment compared with women who had inactive treatment. The review was last published in 2008 and declared as stable not to be further updated.
For relief of overall pain, there may be a slight decrease in favour of treatment with GnRHas compared to placebo or oral or injectable progestogens. We are uncertain about the effect when comparing GnRHas with danazol, intra‐uterine progestogens or gestrinone. For bone-mineral density (BMD), there may be a slight decrease when women are treated with GnRHas, compared to gestrinone. There was a bigger decrease of BMD in favour of GnRHas, compared to GnRHas in conjunction with calcium‐regulating agents. However, there may be a slight increase in adverse effects when women are treated with GnRHas, compared to placebo or gestrinone. Due to a very low to low certainty of the evidence, a wide range of outcome measures and a wide range of outcome measurement instruments, the results should be interpreted with caution.
Progestagens and anti‐progestagens are some of the hormonal drugs used for treatment of pain in endometriosis. This systematic review published in 2012 found limited evidence for the effectiveness of these drugs in the reduction of pain in women with endometriosis. This was due to the limited number of randomised controlled trials comparing each drug. There was no evidence of a benefit of depot or oral progestagens over other treatment. There was no evidence of a benefit of anti‐progestagens. Data should be interpreted with caution due to the limited number of trials and small sample sizes. An update of the review is currently in development.
Progesterone receptor modulators have been advocated as one of the hormonal treatments for endometriosis. Mifepristone may relieve dysmenorrhoea (painful periods) and dyspareunia (pain during sexual intercourse) compared to placebo in women with endometriosis. However, amenorrhoea (absence of menstrual periods) and hot flushes were common side effects of mifepristone. Evidence was insufficient to show differences in rates of nausea, vomiting, or fatigue, if present. Some studies assessed other progesterone receptor modulators. Researchers compared gestrinone versus other treatments (danazol or leuprolin), ulipristal versus leuprolide acetate, and asoprisnil verus placebo. However, evidence was insufficient to allow firm conclusions regarding the safety and effectiveness of these interventions. An update of the review is currently in development.
The combined oral contraceptive pill (COCP) is commonly used to treat pain associated with endometriosis but how well it works is unclear. This review looked at two main comparisons:
-Combined oral contraceptive pill versus placebo
-Combined oral contraceptive pill versus other medical treatment (goserelin)
The quality of the evidence was very low. There was insufficient evidence to make a judgement on the effectiveness of the COCP compared with other medical treatments.
The review published in 2008 concluded that hormone replacement therapy for women with endometriosis and post‐surgical menopause could result in pain and disease recurrence. However, the evidence in the literature was not strong enough to suggest depriving severely symptomatic patients from this treatment in order to relieve their menopausal symptoms. There is a need for double‐blinded randomised controlled studies to investigate further the effects of hormone replacement therapy on disease and pain recurrence.
Studies support the contributing role of inflammation in endometriosis‐related pain. Since anti‐TNF‐α drugs can inhibit the inflammation process, it is hypothesised they could relieve the symptoms of the disease without inhibiting ovulation. However, this systematic review included only one randomised controlled trial and found that there was not enough evidence from which to draw conclusions about the effectiveness and safety of anti‐TNF‐α drugs in relieving pain in women with endometriosis. The review was declared as stable in 2013.

Nonsteroidal anti‐inflammatory drugs (NSAIDs) are readily available without prescription for pain relief. They work by preventing or slowing down the production of prostaglandins, which helps to relieve the painful cramps associated with endometriosis. Authors conducted this review to compare effectiveness and safety of NSAIDs for painful symptoms caused by endometriosis versus placebo, other pain management drugs or no treatment. The review found very limited evidence on the effectiveness of NSAIDs (specifically naproxen) for management of pain caused by endometriosis (1 trial with 24 women). In 2017 the review was declared as stable as authors did not identify any new or ongoing studies and concluded that more studies are unlikely.
Medical treatment aims to relieve symptoms and shrink lesions by suppressing the normal menstrual cycle. In this 2021 review, authors considered medication specifically aiming to modulate oestrogen receptors. Only one randomised controlled trial was included in the review. This study compared the SERM 'raloxifene' versus placebo in 93 women who had undergone complete surgical excision of all endometriosis lesions. Based on the single study included in this review, reviewers found no evidence of a beneficial effect of SERMs as treatment for pain relief in surgically treated endometriosis. On the contrary, the study was prematurely stopped because women who used SERMs experienced a return of pain sooner than women who used placebo.
Post-surgical medical treatment
The progestogen levonorgestrel is a hormonal medication that is believed to stop the growth of endometrial tissue outside the womb. The aim of this review was to assess whether the use of a hormone‐releasing intrauterine device (LNG‐IUD ) was beneficial for managing associated painful symptoms and improving the quality of life and patient satisfaction in women who have recently had surgery for endometriosis. At this stage, there is not enough evidence to support the use of LNG‐IUD after surgery to reduce pain caused by endometriosis. Although there was some evidence of a benefit in reducing painful periods and improving quality of life and satisfaction when using LNG‐IUD after surgery, the certainty of evidence was low to very low, due to the small numbers of studies and study participants, as well as flaws in study design. This suggests that further studies are required before a recommendation can be made for its use.
Alternative treatments

This review examined the effectiveness of acupuncture for reducing pain in endometriosis; however only one study met the inclusion criteria. The data from the included study, involving 67 women, indicated that ear acupuncture was more effective compared to Chinese herbal medicine for reducing menstrual pain. The study did not report whether participants suffered any side effects from their treatments. Larger, well‐designed studies comparing acupuncture with conventional therapies are necessary to confirm these results. An update of the review is in development.
The two small studies in this review suggest that Chinese herbal medicine (CHM) may be as effective as gestrinone and may be more effective than danazol in relieving endometriosis‐related pain, with fewer side effects than experienced with conventional treatment. However, the two trials included in this review were small and of limited quality so these findings must be interpreted cautiously. Better quality randomised controlled trials are needed to investigate a possible role for CHM in the treatment of endometriosis. An update of the review is in development.
Reviews reporting fertility outcomes

Medical treatment
Many women affected by endometriosis suffer with infertility and may, as a result, seek in vitro fertilisation (IVF) or intracytoplasmic sperm injection (ICSI) treatment. IVF/ICSI is known to be less successful in women with endometriosis and a variety of interventions prior to IVF/ICSI have been proposed to try and improve outcomes including long-term gonadotrophin-releasing hormone (GnRH) agonist therapy before IVF for pituitary down‐regulation. Compared to no pretreatment, we are uncertain whether long‐term GnRH agonist therapy prior to IVF/ICSI in women with endometriosis affects live birth rate, complication rate, clinical pregnancy rate, multiple pregnancy rate and miscarriage rate.
Pentoxifylline is an immunomodulator (a substance that has an effect on the immune system) that might offer an alternative approach for treating this condition. The review published in 2021 included 5 randomised controlled studies. There was not enough evidence to permit any conclusions about the effectiveness and safety of pentoxifylline in terms of fertility and pain relief outcomes in women with endometriosis. No studies reported on the primary outcome of live birth rate or on adverse events (side effects).
Endometriosis is an estrogen-dependent disease. For many years, the use of drugs such as danazol to stop ovulation and the production of estrogen has been standard practice in the treatment of pain and subfertility caused by endometriosis. This works well for pain, but does not appear to improve fertility. In fact, as ovulation and periods are stopped for the time of treatment, fertility may be reduced by this approach. Authors concluded there was no evidence of benefit with the use of ovulation suppression for women with endometriosis and infertility. In 2009 the review was declared as stable.
Surgical interventions

Endometriosis can cause pain, infertility, and other symptoms which can reduce quality of life. One available treatment for endometriosis is laparoscopic or 'keyhole' surgery, performed to remove visible areas of endometriosis. A keyhole surgery includes excision (cutting a lesion out) and/or ablation (destruction of the lesion by burning). In 2020, Cochrane authors assessed the evidence on the use of laparoscopic surgery to treat pain and infertility in women with endometriosis. No data were reported on live birth. Laparoscopic surgery probably increases pregnancy rate compared to diagnostic laparoscopy. It is uncertain if laparoscopic surgery reduces ectopic pregnancy rate and miscarriage rate compared to diagnostic laparoscopy. Compared to diagnostic laparoscopy, it is uncertain whether laparoscopic surgery reduces overall pain associated with endometriosis. There was insufficient evidence on adverse events to allow any conclusions to be drawn regarding safety. An update of the review is in development.
Endometriomata are benign growths of the ovary. Evidence suggests that surgery to remove the endometrioma provides better results than draining and destroying the lining of the cyst with regard to the recurrence of the cyst, pain symptoms and also the chance of a spontaneous pregnancy in women who were previously subfertile. Evidence that one technique is favoured in women who desire to conceive and who seek in vitro fertilization (IVF) treatment is however lacking. An additional randomised trial demonstrated that in women trying to conceive the ovarian response to stimulation, as part of fertility treatment, is better in women who have undergone surgery to remove the cyst rather than draining and destroying the endometrioma. The subsequent likelihood of pregnancy was not affected. Further research is required in this field to assess quality of life after surgery, clarify the effect of surgery on fertility with IVF treatment and to study the effect of surgery on ovarian function. An update of the review is in development.
Medical and surgical interventions
Common treatments of endometriosis are hormonal suppression with medical therapy to reduce the size of endometriotic lesions or laparoscopic surgery (where small incisions are made in the abdomen) to remove visible areas of endometriosis. Though the combination of surgery and medical therapy appears to be beneficial, there is a lack of clarity about the appropriate timing of when medical therapy should be used in relation with surgery, that is, before, after, or both before and after surgery, to maximize treatment response. Cochrane authors updated the review in 2020. They concluded that the data about the efficacy of medical therapy for endometriosis are inconclusive, related to the timing of hormonal suppression therapy relative to surgery for endometriosis. In the various comparisons of the timing of hormonal suppression therapy, women who receive postsurgical medical therapy compared with no medical therapy or placebo may experience benefit in terms of pain recurrence, disease recurrence, and pregnancy. There is insufficient evidence regarding hormonal suppression therapy at other time points in relation to surgery for women with endometriosis.
Endometriomata are a form of ovarian endometriosis, classified as cysts within the ovaries. They are a common cause of subfertility and pelvic pain. This review aimed to determine which treatment approach was better for women with subfertility and endometriomata who were undergoing assisted reproductive technology (ART). Four trials were identified. A gonadotropin-releasing hormone (GnRH) agonist showed a positive treatment effect on the ovarian response to controlled ovarian hyperstimulation (COH) and the number of mature oocytes retrieved compared to GnRH antagonist. The evidence for surgery was limited but aspiration was associated with a greater ovarian response than expectant management (a wait and see approach). Further randomised controlled trials of interventions for the management of endometrioma in women undergoing ART are required.
Diagnostic test accuracy (DTA) reviews
Currently, the only reliable way of diagnosing endometriosis is to perform laparoscopic surgery and visualise the endometrial deposits inside the abdomen. Because surgery is risky and expensive, imaging tests have been assessed for their ability to detect endometriosis non‐invasively. A DTA review published in 2016 concluded that none of the imaging methods was accurate enough to provide this information on overall pelvic endometriosis. Transvaginal ultrasound identified ovarian endometriosis with enough accuracy to help surgeons determine whether surgery was needed, and magnetic resonance imaging (MRI) was sufficiently accurate to replace surgery in diagnosing endometrioma but was evaluated in only a small number of studies. Other imaging tests were assessed in small individual studies and could not be evaluated in a meaningful way. Transvaginal ultrasound could be used to locate more anatomical sites of deep endometriosis when compared with MRI, helping surgeons better plan an operative procedure. Endometriosis in the lower bowel appears to be relatively accurately identified by both transvaginal and transrectal ultrasound, by MRI and by multi‐detector computerised tomography enema. New types of ultrasound and MRI show a lot of promise in detecting endometriosis, but studies are too few to clearly show their diagnostic value. Additional high‐quality research is needed to accurately evaluate the diagnostic potential of non‐invasive imaging tests for endometriosis. An update is currently under development.
Authors evaluated whether the results of blood tests (blood biomarkers) can help to detect endometriosis non‐invasively. Only four of the assessed biomarkers (anti‐endometrial Abs (anti‐endometrial autoantibodies), interleukin‐6 (IL‐6), CA‐19.9 and CA‐125) were evaluated by enough studies to provide a meaningful assessment of test accuracy. None of these tests was accurate enough to replace diagnostic surgery. Several studies identified biomarkers that might be of value in diagnosing endometriosis, but there are too few reports to be sure of their diagnostic benefit. Overall, there is not enough evidence to recommend testing for any blood biomarker in clinical practice to diagnose endometriosis. More high-quality research trials are necessary to accurately assess the diagnostic potential of certain blood biomarkers, whose diagnostic value for endometriosis was suggested by a limited number of studies.
An accurate urine test could lead to the diagnosis of endometriosis without the need for surgery. Can any urine test be accurate enough to replace or reduce the need for surgery in the diagnosis of endometriosis? None of the assessed biomarkers, including cytokeratin 19 (CK 19), enolase 1 (NNE), vitamin D binding protein (VDBP) and urinary peptide profiling have been evaluated by enough studies to provide a meaningful assessment of test accuracy. None of the tests were accurate enough to replace diagnostic surgery. Several studies identified biomarkers that might be of value in diagnosing endometriosis, but there are too few reports to be sure of their diagnostic benefit. There is not enough evidence to recommend any urinary biomarker for use in clinical practice for the diagnosis of endometriosis. More high-quality research trials are needed to accurately assess the diagnostic potential of urinary biomarkers identified in small numbers of studies as having value in detecting endometriosis.
Can physicians use biomarkers (distinctive molecules, genes or other characteristics that appear in certain conditions) to reduce the need to surgically diagnose endometriosis? Only two of the assessed biomarkers, a neural fibre marker PGP 9.5 and hormonal marker CYP19, were assessed in sufficient number of studies to obtain meaningful results. PGP 9.5 identified endometriosis with enough accuracy to replace surgical diagnosis. Several additional biomarkers (endometrial proteome, 17βHSD2, IL‐1R2, caldesmon and other neural markers) show promise in detecting endometriosis, but there are too few studies to be sure of their diagnostic value. Further high-quality research is necessary to accurately evaluate the diagnostic potential of the endometrial biomarkers for the diagnosis of endometriosis.
In this review, fifteen combinations of different blood, endometrial and urinary biomarkers were studied, incorporating ultrasound, clinical history, and examination. Each combination of tests was assessed in small individual studies. Several studies identified the combined tests that might be of value in diagnosing endometriosis, but there are too few reports to be sure of their diagnostic benefit. The reports were of low methodological quality, which is why these results cannot be considered reliable unless confirmed in large high‐quality studies. Overall, there is not enough evidence to demonstrate benefit of any combined non‐invasive test for use in clinical practice for the diagnosis of endometriosis over the current ‘gold standard’ of diagnostic laparoscopy. More high‐quality research studies are needed to accurately assess the diagnostic potential of any type of non‐invasive tests or their combinations that were identified in only a few studies as possibly having value in the detection of endometriosis.
Protocols
Objective: To determine the effectiveness and safety of GnRH antagonists in the treatment of pain associated with endometriosis. The review is currently in editorial.
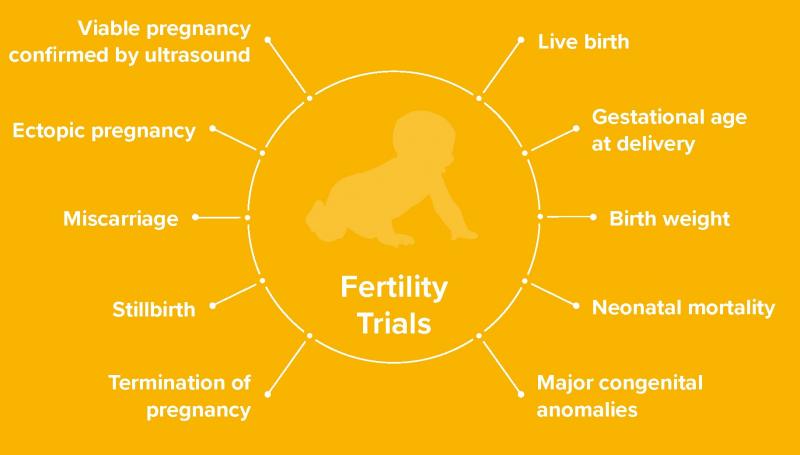
A core outcome set for future endometriosis research
Research studies testing new treatments for endometriosis often measure different outcomes. For example, when a new medicine is being tested, one researcher may decide to measure overall pain (an outcome) and another researcher may only measure medicine side effects (a different outcome). When the two studies are finished, the results from both studies cannot be easily compared or combined to see which treatment works best. This is a barrier to improving the care women with endometriosis receive. The endo:outcomes collaboration has brought together healthcare professionals, researchers, and women with endometriosis to overcome this barrier. Using formal consensus methods, over 300 people from 29 countries have developed a core set of outcomes that should be collected and reported by future endometriosis research.
The collaboration anticipates these core outcomes, developed to specifically highlight the outcomes perceived as most important by healthcare professionals, researchers, and women with endometriosis, will assist funding organisations to prioritise research funding, help researchers to design future research, and improve the reporting of research in medical journals.

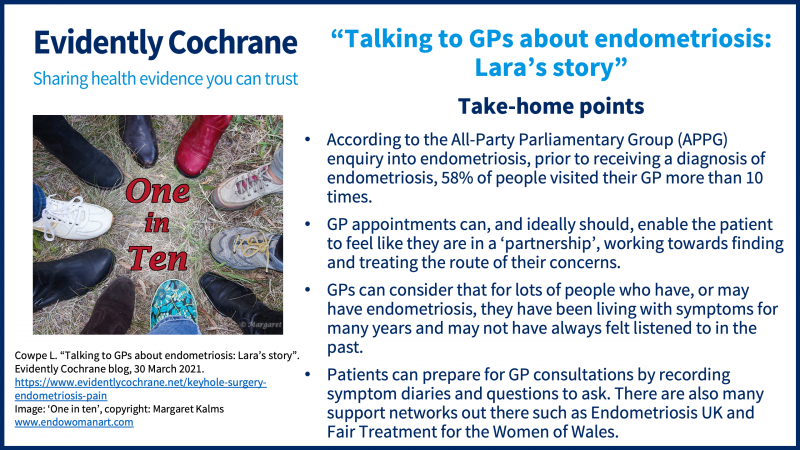
Throughout #EndometriosisAwarenessMonth we have also shared blogs that included relevant Cochrane evidence and other information to help inform women’s decisions about endometriosis diagnosis and treatment.
Dr James Duffy discussed the Cochrane evidence on blood tests for diagnosing endometriosis.
Dr Mathew Leonardi and Dr James Duffy discussed the latest Cochrane evidence on the use of ultrasound to diagnose endometriosis.
Dr Sarris and Dr Duffy discussed how endometriosis can impact fertility, potential treatment options, the latest Cochrane evidence on keyhole surgery for endometriosis.
Claire Barker shared her experiences of using hormonal contraceptives for her endometriosis pain, and Dr Hirsch discussed the latest Cochrane evidence.
Lara Cowpe reflected upon her experiences with GPs during her endometriosis journey.